CHIEF COMPLAINTS:
Patient came to the hospital with the chief complaints of - fever , headache , altered sensorium.
HOPI:
Patient was apparently asymptomatic 5 days back, then he developed,
High grade fever which was acute in onset associated with chills , intermittent in nature, relieved on medication and was associated with headache.
Altered sensorium since 2 to 3 hours (not talking and not working properly)
No history of burning micturition, vomiting, loose stools, SOB, cough ,chest pain, bleeding manifestations.
PERSONAL HISTORY:
Diet- mixed
Appetite- Normal
Sleep - adequate
Bowel - regular
Bladder - Normal
Patient is an occasional drinker but stopped 1 month back.
PAST HISTORY:
N/K/C/O DM ,HTN,BA,TB, CVA,CAD, epilepsy
ADDICTIONS:
No significant drug history
FAMILY HISTORY : not significant
GENERAL EXAMINATION: Prior Consent was taken.
Patient is oriented to time ,place and person
Poorly built and poorly nourished.
Examined in a well lit room.
No Pallor /Icterus /Cyanosis/clubbing/Edema of feet /Lymphadenopathy.
VITALS :
Temp : 101 F
PR : 90 bpm
BP : 140/80 mmhg
RR : 18
SPO2 : 98 % at RA
GRBS-122 mg/dl
SYSTEMIC EXAMINATION :
CARDIOVASCULAR SYSTEM : S1 and S2 heard, no murmurs heard .
RESPIRATORY SYSTEM : Bilateral air entry present , clear .
PA : soft and non tender
CNS:
GCS-
E4V3M6, on Day 1
pupils- B/L NSRL
HIGHER MENTAL FUNCTIONS:
- Oriented to time,place,person
- Memory : immediate,recent, remote intact
- Speech: normal
- No delusions or hallucinations
CRANIAL NERVES:
1- normal
2- visual acuity - normal
3,4,6- No restriction of movement of eye
5-normal( muscles of mastication+sensations of face)
7- normal
8- Normal hearing
9,10- No difficulty in swallowing and speech, gag reflex not tested
11,12- normal.
MOTOR SYSTEM EXAMINATION :
TONE: normal
POWER : Right Left
Upper limb 5/5 5/5
Lower limb 5/5 5/5
Reflexes : Right Left
- Biceps: 2+ 2+
- Triceps: 2+ 2+
- Supinator: 2+ 2+
- Knee: 2+ 2+
- Ankle: 2+ 2+
Plantars: flexor flexor
Meningeal signs-
Neck stiffness -present on Day 1 and 2
Decreased on Day 6
Kernigs sign - positive on day 1 and 2
Absent on day 6
SENSORY EXAMINATION:
Crude touch. + +
Pain. + +
Temp. + +
Fine touch-- present
Vibration. + +
Position. + +
CEREBELLUM EXAMINATION:
- Able to do finger nose test.
- Dysdiadokinesia present on day 2
- No rebound tenderness
- Gait: Normal
- Romberg's sign: Negative
AUTONOMIC NERVOUS SYSTEM:
- No abnormal sweating
- No resting tachycardia
MRI Impression on day 1:
- Few lacunar infarcts in medulla on left side.No f/o raised ICT on MRI
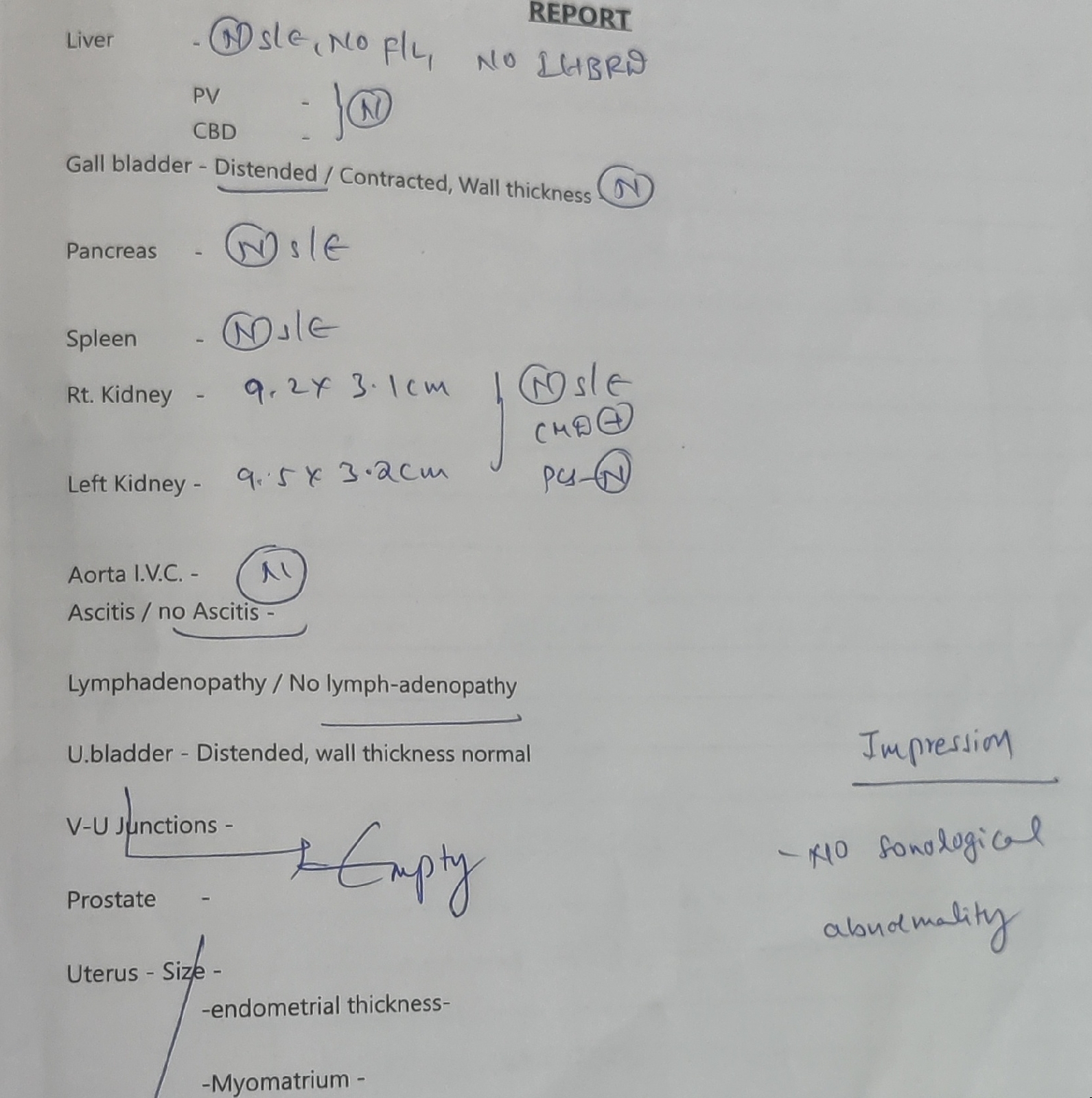
Ultrasound report on day 1;
Opthal- fundoscopy i/v/o any raised ICT for LP
Investigations on Day 1:
Blood culture report on day 3
Urine culture report on day 3
LUMBAR PUNCTURE: On Day 1:
LP done on 24-3-22 at 2 am - showing around 450 cells? Lymphocyte predominant,
Glucose - 32
Protein - 195
Chloride - 120
GRBS at time of LP - 112mg/dl
TREATMENT:
On Day 1;
IVF NS ,RL ,DNS@100 ml/hr
INJ PANTOP 40 MG IV/OD
INJ.NEOMOL 1 GM IV SOS
INJ. MONOCEF 2 GM IV BD
INJ. DEXA 8 MG IV STAT
TAB DOLO 650 MG RT/SOS
BP,PR monitoring 4 th hourly
On Day 2:
IVF NS ,RL ,DNS@100 ml/hr
INJ PANTOP 40 MG IV/OD
INJ.NEOMOL 1 GM IV SOS if temp >101°F
INJ.Thiamine 1 amp in 100ml NV/IV/OD
INJ. MONOCEF 2 GM IV BD
INJ. DEXA 4 MG IV STAT
INJ DOXY 100 mg IV BD
Strict I/O charting
W/f seizure activity
INJ. Vancomycin 2mg IV stat
INJ.Optineuron 1amp + 500ml NS over 1hr
BP,PR monitoring 4 th hourly
On Day 3:
IVF NS ,RL ,DNS@100 ml/hr
INJ PANTOP 40 MG IV/OD
INJ.NEOMOL 1 GM IV SOS
INJ.Thiamine 1 amp in 100ml NV/IV/OD
INJ. MONOCEF 2 GM IV BD
INJ. DEXA 4 MG IV STAT
INJ DOXY 100 mg IV BD
TAB DOLO 650 pO TID
Strict I/O charting
W/f seizure activity
INJ. Vancomycin 1mg IV BD
INJ.Optineuron 1amp + 500ml NS over 1hr
BP,PR monitoring 4 th hourly
On Day 4:
IVF NS ,RL ,DNS@100 ml/hr
INJ PANTOP 40 MG IV/OD
INJ.NEOMOL 1 GM IV SOS
INJ.Thiamine 200mg IV BD
INJ. MONOCEF 1 GM IV BD
INJ. DEXA 4 MG IV BD
INJ DOXY 100 mg PO BD
TAB DOLO 650 pO TID
Strict I/O charting
W/f seizure activity
INJ. Vancomycin 1mg IV BD
INJ.Optineuron 1amp + 100ml NS over 1hr
BP,PR monitoring 4 th hourly.
On Day 5:
IVF NS ,RL ,DNS@100 ml/hr
INJ PANTOP 40 MG IV/OD
INJ.NEOMOL 1 GM IV SOS
INJ.Thiamine 200mg IV BD
INJ. MONOCEF 1 GM IV BD
INJ. DEXA 4 MG IV BD
INJ DOXY 100 mg PO BD
TAB DOLO 650 pO TID
Strict I/O charting
W/f seizure activity
INJ. Vancomycin 1mg IV BD
INJ.Optineuron 1amp + 100ml NS over 1hr
BP,PR monitoring 4 th hourly.
Provisional diagnosis- meningitis?
Reference log:
https://divyaraju26.blogspot.com/2022/03/47-year-old-male-with-fever-headache.html
Popular posts from this blog
56-year-old patient with generalised weakness, fever, shortness of breath and cough
August 31st, 2021 CHENNAMADHAVUNI DIVYA, 9th semester Roll number-21 This is an online E logbook to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from an available global online community of experts to solve those patients clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box are welcome. I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan. Following is the view of my case: Date of admission :- 28-8-2021 Chief complaints : A 56-year-old male patient has come to the opd with th
36 year old male with epigastric pain.
36 year old male with epigastric pain This is an online e logbook to discuss our patients deidentified health data shared after taking her/guardian's signed informed consent Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs This E log also reflects my patient centre’s online learning portfolio and valuable inputs on the comment box is welcom e. Case History CHIEF COMPLAINTS - A 36 year old male , driver by occupation ,came to the casualty with cheif complaints of -P ain in the epigastric region since 9 days HISTORY OF PRESENTING ILLNESS - Patient was apparently asymptomatic 9 days back h/o complains of epigastric pain on 1st of janunary Type- Continuous,dragging type of pain Non radiating. Onset - sudden Duration - since 9 days Aggrevated by sleeping in lateral position. Relieved on medications. Associ
- Get link
- X
- Other Apps
- Get link
- X
- Other Apps

















Comments