MEDICINE CASE DISCUSSION:
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
A 40 YEAR OLD FEMALE WITH SHORTNESS OF BREATH AND FEVER
CASE:
A 40 year old female came with the complaints of
*fever since the past 20 days
*shortness of breath since the past 3 days
*vomiting for the past 1 day
*decreased urine output for the past 1 day.
HER DAILY ROUTINE:
Patient was a daily wage worker by occupation. She starts her day at 4am and finishes her morning routine by 6am. She consumes alcohol daily, around 750 ml for the last five years which began after her husband passed away.
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 20 days ago, when she had an insidious onset of intermittent fever which was low grade, with an evening rise in temperature. This was associated with chills and rigours, and was relieved on taking medications.
The fever was non relenting, so she was admitted to a local hospital in miryalaguda 3 days back where she was given conservative therapy with antibiotics and analgesics, and then she was referred to our hospital 1 day back.
The patient has been complaining of shortness of breath for the past 20 days. Shortness of breath is present while doing daily activities- Grade 3 (Ex. Washing clothes, cleaning utensils) which gradually progressed to the current state, where the patient has shortness of breath even at rest (Grade 4). This was not associated with orthopnoea, paroxysmal nocturnal dyspnea or pedal edema.
The patient has had two episodes of vomiting which are non projectile, non bilious, non foul smelling , non- blood stained and contains undirected food particles.
Patient has had decreased urine output from the past 1 day, associated with burning micturition.
Patient has visual hallucinations, self-talking and irrelevant talking ( under evaluation)
No associated abdominal pain, constipation, diarrhoea, melaena.
PAST HISTORY:
Medical history-
The patient is not a known case of Diabetes Mellitus, tuberculosis, asthma, epilepsy, CAD
She had been diagnosed with hypertension 3 years ago, for which she is not on any medication.
Surgical history-
There is no relevant surgical history for this patient
PERSONAL HISTORY:
Appetite- Decreased since the past 20 days
Diet- Vegetarian
Sleep- Decreased since past 20 days
Bowel and Bladder movements- Urine output decreased for past 1 day, Stools-passed 2days back )
Addictions- Patient consumes alcohol daily for the past five years (750ml per day for the past five years)
She also has a habit of tobacco chewing occasionally for past 2 years.
Menstrual History:
Menarche-12 years
Cycle repeats for every 28 days
She bleeds for 5 days, 5 pads per day, no clots
Family history- not significant
GENERAL EXAMINATION:
With prior consent, patient was examined in a well lit room, lying down comfortably on the bed
The patient was conscious, coherent, and co-operative and well oriented to time, place and person. . She in thin built and moderately nourished.
Pallor- Present
Icterus- Present
Clubbing- Absent
Cyanosis- Absent
Lymphedenopathy- Absent
Edema- Absent
Kolionychia- Absent
VITALS-
Temperature- 98.4 F
Pulse rate- 110 bpm
Blood pressure- 110/70 mmHg
Respiratory rate- 36 cpm
Sp02 at room temp- 95%
SYSTEMIC EXAMINATION:
Abdominal examination-
INSPECTION:
Shape – scaphoid, not distended
Flanks – free
Umbilicus – Central, inverted
Skin- LSCS scar is present, no sinuses, striae are seen
Dilated veins – absent
No visible gastric peristalsis or intestinal peristalsis
PALPATION:
Superficial Palpation –
No local rise of temperature or tenderness
Deep Palpation-
Liver-
It is palpable in the Right hypochondrium about 5 cms below the Right costal margin in the Mid clavicular line and 2 cms in the midline from the Xiphisternum, which moves with respiration and is firm in consistency with a Smooth surface and a rounded edge. The upper border of the liver is not palpable.
Spleen-
Spleen is palpable in the Left Hypochondrium, enlarging towards the Right Iliac Fossa,2 cms below the Left Costal Margin in the Mid clavicular line, which moves with respiration and is firm in consistency with a Smooth surface and a rounded edge.
Kidney:
It is not palpable
No other Palpable swellings in the abdomen.
PERCUSSION:
Percussion of Spleen- Dull note on percussion
There is no fluid thrill, shifting dullness
AUSCULTATION:
Bowel sounds are heard
RESPIRATORY SYSTEM-
Inspection-
Chest is bilaterally symmetrical
The trachea is positioned centrally
Apical impulse is not appreciated
Chest moves normally with respiration
No dilated veins, scars or sinuses are seen
Palpation-
Trachea is felt in the midline
Chest moves equally on both sides
Apical impulse is felt in the fifth intercostal space
Tactile vocal fremitus- appreciated
Percussion-
The areas percussed include the supraclavicular, infraclavicular, mammary, inframammary, infraaxillary, suprascapular, infrascapular, interscapular areas.
They are all resonant.
Auscultation:
B/l air entry- present
NVBS are heard. No adventitious sounds were heard.
CVS-
Inspection-
The chest wall is bilaterally symmetrical
No dilated veins, scars or sinuses are seen
Apical impulse or pulsations cannot be appreciated
Palpation-
Apical impulse is felt in the fifth intercostal space, 2 cm away from the midclavicular line
No parasternal heave or thrills are felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
CNS-
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system
BULK Right. Left
Upper limbs N N
Lower limbs N N
TONE
Upper limbs N N
Lower limbs N N
POWER
Upper limbs 5/5 5/5
Lower limbs 5/5 5/5
Superficial reflexes and deep reflexes are present , normal
Gait- Could not elicit, the patient was not able to get off the bed
No involuntary movements
Sensory system - All sensations (pain, touch, temperature, position, vibration sense) are well appreciated.
INVESTIGATIONS:
On 12/1/22:
PH- 7.40
PC02- 21.3
P02- 54.7
HC03- 13.0
Serum LDH- 346 IU/L
LFT-
Total bilirubin- 4.7 mg/dl
Direct bilirubin- 2.57 mg/dl
AST- 102
ALT- 35
ALP- 144
Total proteins- 5.6
Albumin- 2.3
A/G- 0.72
RFT-
Urea- 45 mg/dl
Creatinine- 3.2
Uric acid- 8.0
Ca- 10 mg/dl
Na- 136
P- 4.4 mg/dl
K- 4.8 meq/lt
Cl- 90 meq/lt
Coagulation profile-
PT- 20
INR- 2.4
aPtt- 41
Complete urine examination-
Albumin- ++
Sugar, bile salts, bile pigments- normal
Pus cells- 10-12
Epithelial cells- 4-5
RBC- 3-4
Casts- granular casts are present
Complete blood picture-
Reticulocyte count- 0.5%
Hb- 5.7
TLC- 18400
N/L/E/M- 93/4/1/2
PLT- 65000
Urine output on 12/1/22:
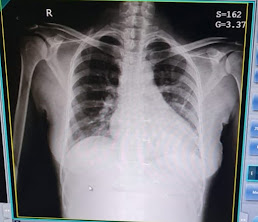
Chest X-ray
2D- Echo:
*Good left ventricular systolic function
*No regional wall motional abnormalities
*Right atria mild dilated
*Sclerotic atrial valve
*Diastolic dysfunction is present.
ECG:
Ultrasound report:
*Hepatosplenomegaly with mildly altered echotexture.
*Mild splenomegaly
*Altered echotexture of renal cortex with well maintained corticomedullary differentiation.
PROVISIONAL DIAGNOSIS:
Fever with hepatosplenomegaly
With anaemia, pre-renal AKI, pre-hepatic jaundice and metabolic acidosis
TREATMENT:
On 11/1/2022:
Rx
1)IVF ons
Urine output +30ml/hr
2)INJ PIPTAZ 4.5 gm*IV*stat
INJ PIPTAZ 2:25gm*IV*TID
3)INJ PAN 40mg*IV*OD
4)INJ ZOFER 4mg *IV*OD
5)GRBS 6th hrly
8am-2pm-8pm-2am
6)strict I/O charting
7)monitor BP/PR/SPo2 monitoring 4th hrly
8)Tab DOXYCYCLINE 100mg*PO*BD
9)INJ FALCFGO 120mg
On 12/1/2022 :
1)IVF 1-NS(urine output+ 30ml/hr)
-RL
2)INJ PIPTAZ 2.25gm*IV*TID
8am-1pm-8pm
3)INJ FALCIGO 120mg*IV
0-12hrs-24hrs-48hrs
4)INJ PAN 40mg*IV*OD
5)INJ ZOFER 4mg*IV*OD
6)GRBS 6th hrly
8am-2pm-8pm-2am
7)strict I/O charting
8)monitor BP/PR/SPo2 chart 4th hrly
9)temp chart 4th hrly
10)syp.cremaffin plus
11)INJ-vit k 10mg/IV stat
12)INJ THIAMINE 1AMP in 100ml NS
Day 4 ( 14/1/22)
S:
Patient is talking irrelavently and agigated behaviour
O:
Patient is drowsy and irritable,
Grbs: 80mg/dl
Bp:110/60mmhg
PR: 94bpm
Spo2: 99%@room air
RR 28
E3 V3 M4
A: cerebral malaria(hepatosplenomagaly)
Sepsis
Severe anemia
Delirium
P:
1.Piptaz 2.25gm/iv/TID
2.Falcigo 120mg/iv
3.Inj zofer 4mg/iv/OD
4.Inj pan 40mg/iv/ OD
5.iv NS (urine output- 30ml/hr)
6. Grbs-6th hrly
15/1/22:
Day 5
S:
Pt Sensorium improved than yesterday
O:
Patient is conscious and oriented
Grbs:120mg/dl
Bp:110/60mmhg
PR: 94bpm
Spo2: 99%@room air
RR 28
Input/output:2500/1100ml
P/A: hepatosplenomegaly+
A: cerebral malaria(hepatosplenomagaly)
Sepsis
Severe anemia
Delirium
P:
1.Piptaz 2.25gm/iv/TID
2.Falcigo 120mg/iv
3.Inj zofer 4mg/iv/OD
4.Inj pan 40mg/iv/ OD
5.iv NS (urine output- 30ml/hr)
6. Grbs-6th hrly






Comments
Post a Comment